Free full-text open-access article: https://doi.org/10.1177/15346501241241540
🙏🙏🙏 Deeply grateful to our hero who this wouldn’t’ve been possible without, Nik Roglić ✨🤝 🙌 🥰
“One of my clients – a nine-year-old, healthy boy – suddenly stopped swallowing even his own saliva, which caused a huge regression in his life. His mouth was constantly full of saliva so he was no longer speaking or using his hands, which were busy holding a napkin in one hand and his lips together with the other. This boy had also stopped participating in activities, was back in nappies, out of school and not sleeping properly.
He had two hospitalizations and the full range of medical work-ups. For 10 days he did not respond to treatment – which is highly unusual. We ended up having to also work with him outside of meals, across his whole day.
The moment when he finally swallowed some saliva, we were all crying and couldn’t believe it. His mum was jumping up and down, hugging him and celebrating. The process took seven weeks but he finally got off his nasogastric tube, gained weight, and reached a variety of 94 foods across food groups.”
➡️From the Blend 4 👉

Abstract
Introduction
- One of the most challenging feeding problems to treat is packing: holding food or liquid in the mouth instead of swallowing. Saliva pooling is most extreme form, a seemingly biological reflexive behaviour.
- Less outwardly apparent than overt aggression or self-injury, but one of the most severe life-threatening problem behaviours, with significant consequences–dehydration, rapid weight loss, adaptive behaviour regression, & hospitalisation, requiring feeding tube placement.
- Original aetiology may be medical or a triggering event, but once resolved, persists for behavioural reasons (avoiding swallowing associated with discomfort or high effort).
- Successful treatment involves graduated exposure with reinforcement to associate swallowing with pleasant experiences & increased success.
- No prior studies on case presentations requiring combined approaches for saliva packing as an undifferentiated automatically-maintained behaviour (the most difficult type to treat) outside of meals without anxiety or saliva expulsion, plus a feeding problem.
Method
- Éloi 9yo, ASD (L3), ID, 100% NG tube dependence, significant adaptive behaviour regression (no longer talking or using his hands or participating in activities, back in nappies, out of school, sleep problems). 10-wks prior during trip overseas, diarrhoea, stopped swallowing (protruding cheeks), hospitalisations & extensive work-up (MRI, endoscopy, blood, faecal/urine, echo, CT; speech, ENT, GI, dental, endocrine, behaviour). 5 teeth pulled, prescribed fibre/laxatives.
- Refused to spit out, didn’t ‘play’ with saliva, no “anxiety,” packed all waking hours and contexts.
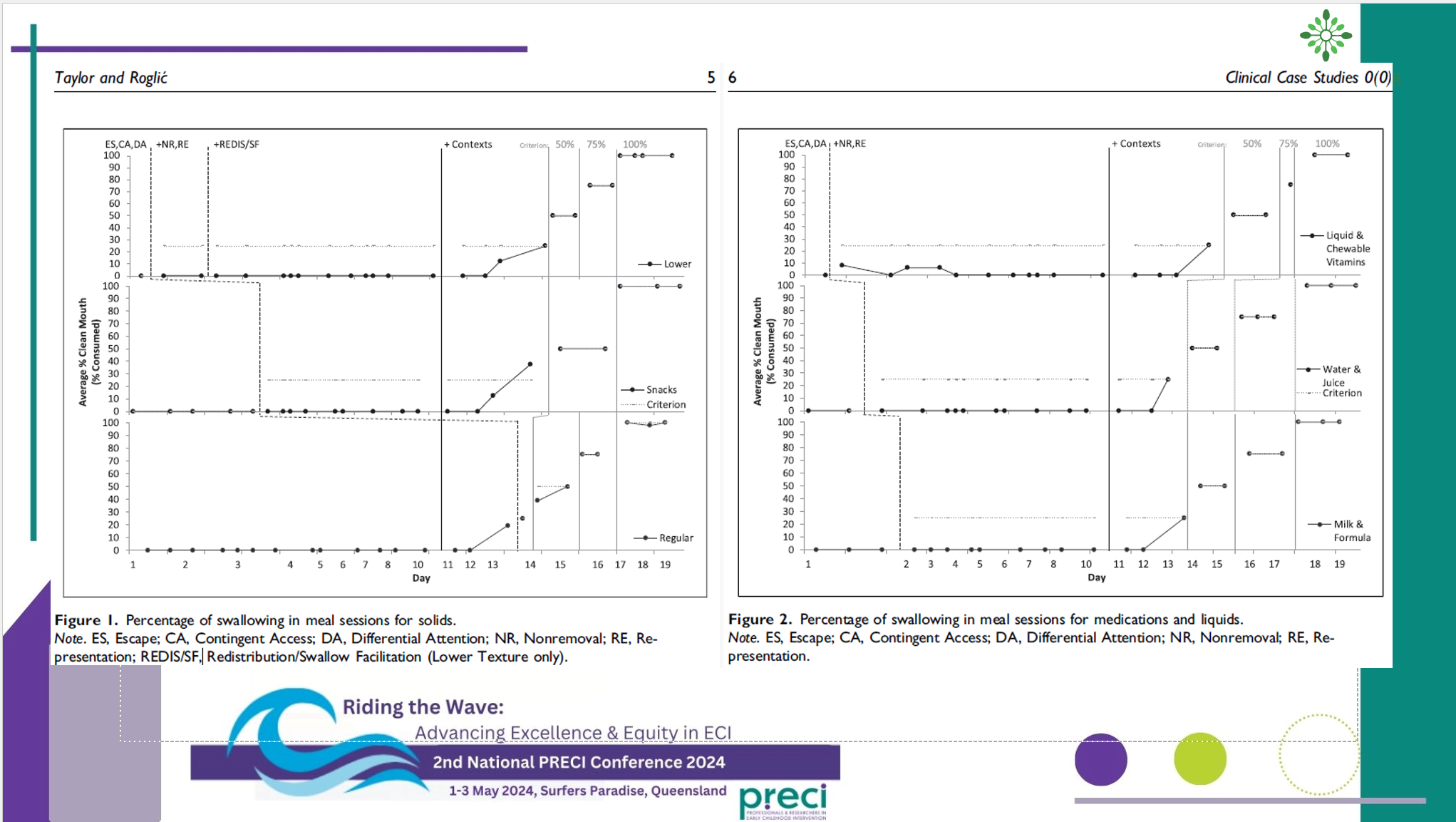
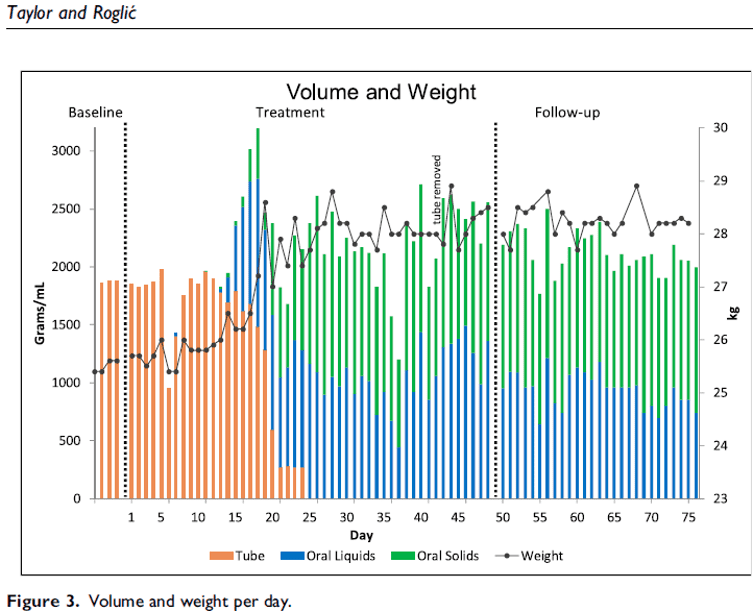
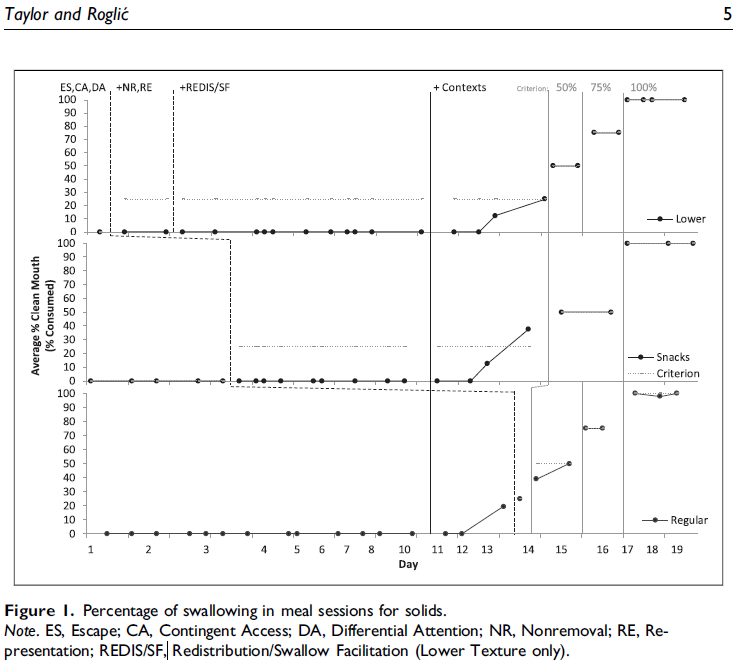
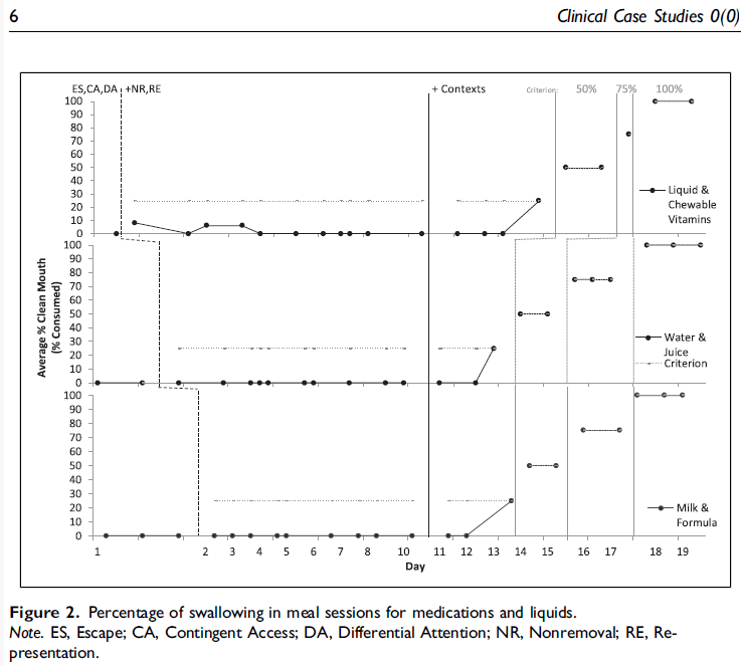
- Intensive 7-week behaviour-analytic paediatric feeding programme. Single-case experimental designs (multiple-baseline, changing criterion). For 10 days, did not respond to typically highly effective specialised feeding interventions & a multitude of treatment probes.
- Saliva packing, as an automatically-maintained undifferentiated behaviour persisting in all waking contexts despite high engagement in activities, warranted an additional/combined feeding & outside of meal approach: structured schedule, all desires put contingent on saliva swallowing, & self-monitoring targeting independence (swallowing saliva without prompting).
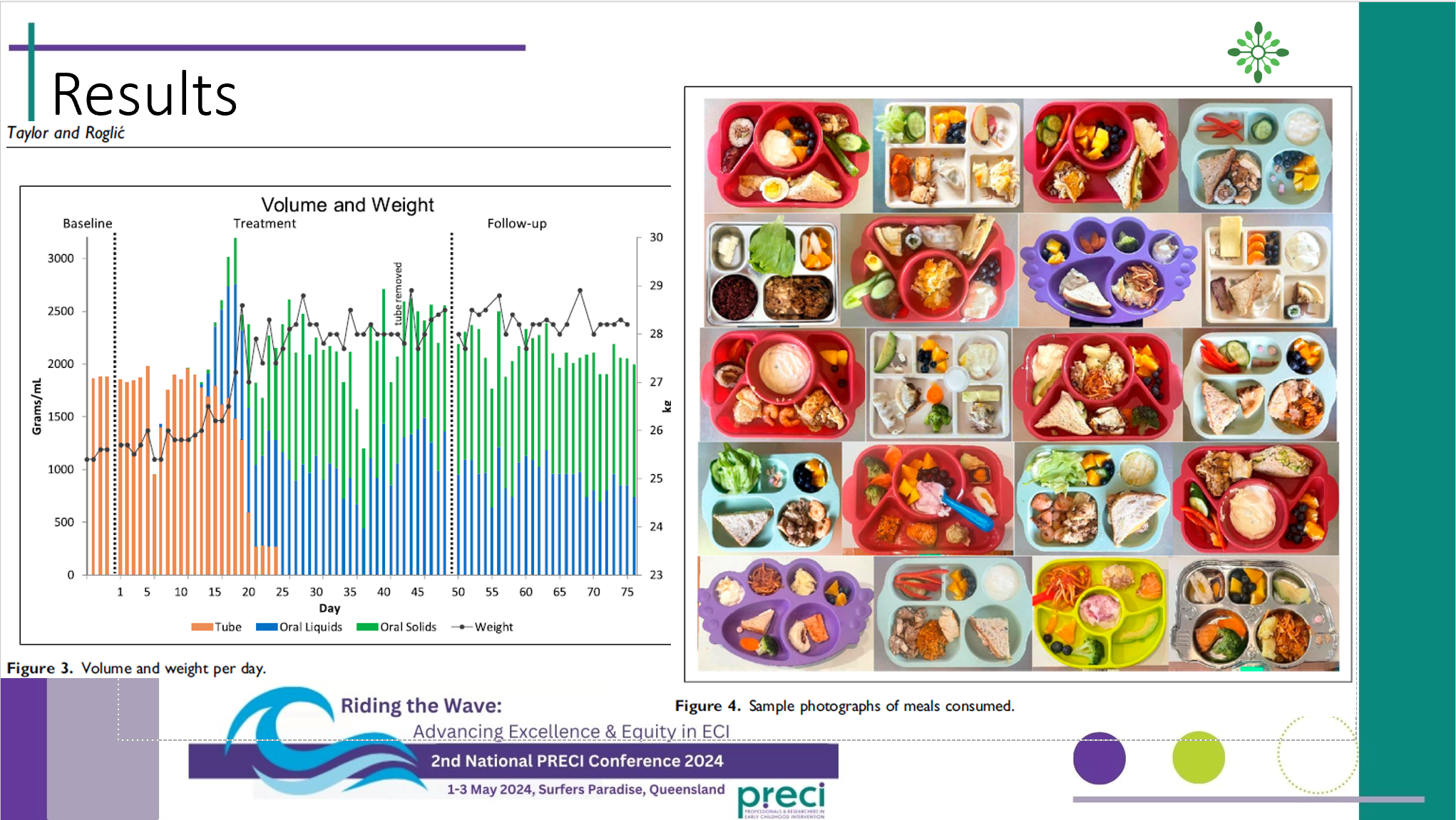
Results
Conclusion
- Met 100% of his 21 goals, gained weight (24.5 to >28kg), eliminated tube dependence (in 23 days). Variety = 94 across all food groups, drinks, & supplements. Caregivers were trained, reported high social validity (all ratings 7/7), gains generalized & maintained in 1-month follow-up. Did not yet reach independence (would not eat/drink or swallow saliva without treatments) due to time/funding constraints.
- First case in Australia of in-home solely behaviour-analytic intervention to eliminate tube dependence, without hunger provocation, weight loss, or limited nutritional variety.
- 🚨📢 Saliva packing may not receive the attention it warrants compared to aggression, self-injury, or other inappropriate mealtime behaviors (eg, throwing, thrashing, spitting). Éloi’s entire broader life & adaptive behavior were significantly disrupted (eg, no longer speaking, in diapers, not using his hands, not going to school, sleeping). Determining severity of pediatric feeding problems, adequate multidisciplinary & medical work-up prior to intervention, & adequate outcomes & procedures requires highly specialized training, expertise, & competence. Children should be referred as early as possible ⏳🧭 to receive expert empirically-supported treatments at the individualized intensity warranted for case severity.