https://doi.org/10.1186/s40337-023-00922-9
There’s lots of talk about ARFID being new and not having an established treatment base. I was really surprised by this at first wondering how they were missing that the pediatric feeding disorder (PFD) treatment literature goes back to the 70s.
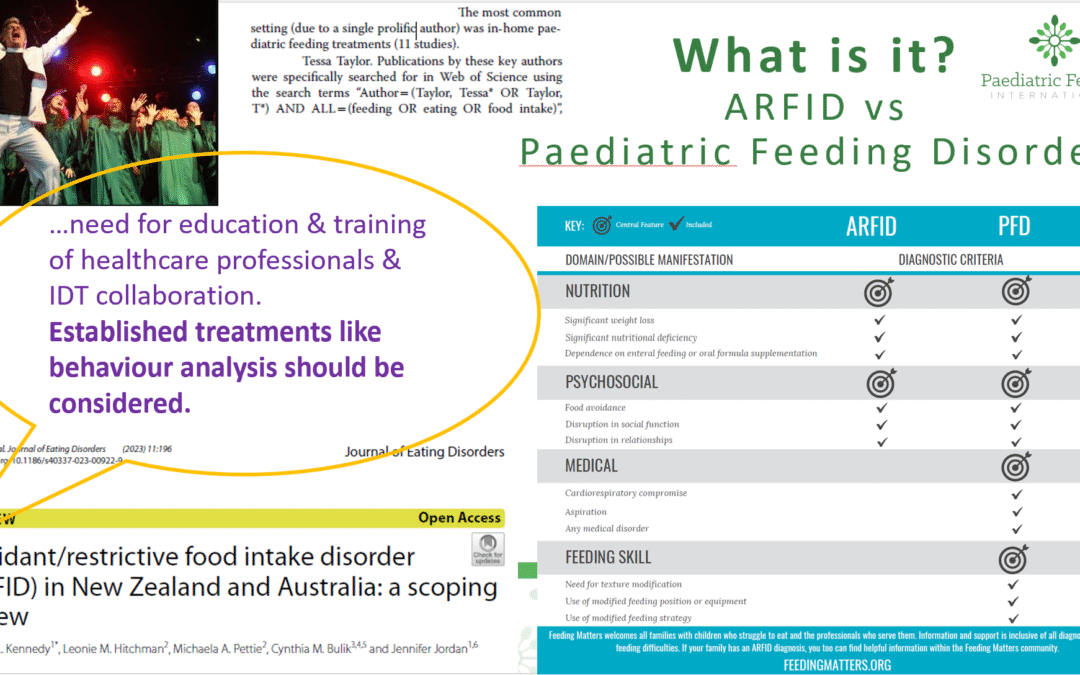
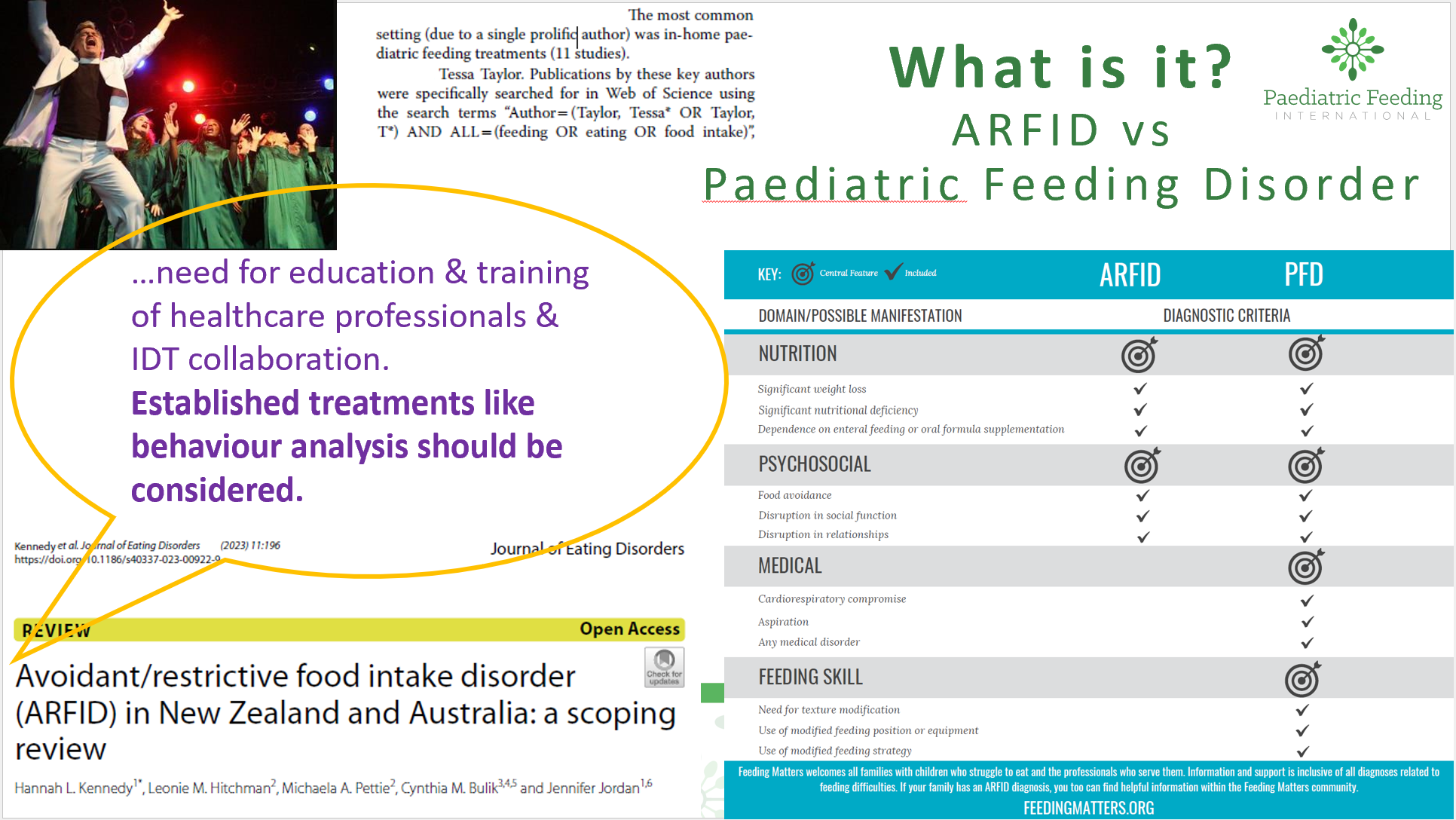
🚨 👏 Writing a review article is already time consuming enough as it is, so I was so happy when the author of this review paper did their ‘homework’ and then some, contacting me to ask if my PFD cases had ARFID (✅) and finally addressed this in print concluding that: 💬 📣there is a need for education and training of healthcare professionals and interdisciplinary team (IDT) collaboration, and that established treatments like behavioral analysis should be considered. Yes, thank you! The article referred to me as a “prolific author” of the most studies in Australia.
We are not wasting worries about what to call it and are more concerned about individualized treatment for each person and families’ mealtime goals than diagnosis. 🧠 👀 If you’re interested in more details about ARFID vs PFD, see our summary below plus the resources we have linked in this post (our lay-friendly article in the Blend mag, our journal publication on successful brief in-home therapy with a teenager, info from Feeding Matters, and our article showing treatment for tube ‘weaning’ working for both CP and ASD). In short, PFD is more comprehensive including skill and medical factors, and younger age. ARFID only includes nutritional and psychosocial impacts. However, a person only needs to meet one criterion for both diagnoses.
Eating or Feeding Disorder? Avoidant/Restrictive Food Intake Disorder (ARFID)? Failure to Thrive/Faltering Growth? Picky Eater? Fussy Eating? Food Selectivity? by Dr. Tessa Taylor
This can be confusing, but names change over time, differ between books and in research, and are mostly unimportant for feeding intervention with an exception: if the person has body image concerns (feelings/worries about their appearance/looks). To simplify, with body image concerns treatment falls under eating disorders (eg, acceptance & commitment therapy/ACT ), but without, under feeding disorders (behaviour-analytic treatment). ARFID is not “new,” but more of a name change on pediatric feeding disorder (PFD) which has more comprehensive criteria (nutrition and psychosocial, plus medical and skill factors). Pediatric feeding disorders already have a well-established empirically-supported treatment (EST) dating back 50 years, so the good thing is you do not need to decide whether it is a disorder or which disorder it is, or if it is severe enough (eg, is it picky or fussy eating or a disorder?). This approach is individualized and simply focuses on each person’s current specific feeding needs and goals (see the checklist) instead of labels. If the feeding problems are mild or caught early, services may just be easier and shorter. It is important to increase awareness of feeding treatment so children without body image concerns get timely evidence-based feeding instead of eating disorder interventions. Although more research is needed with older ages, these treatments can also work outside of pediatrics for individuals without body image concerns, without cognitive or family-based components, medication, or a hospitalization with multiple disciplines. Eating disorder treatments for feeding problems could be unnecessarily complex, costly, ineffective, delay appropriate effective treatments, pose risks (eg, medication side effects), and disrupt quality of life (eg, repeated/lengthy hospital admissions). It is critical to increase awareness of the EST for feeding so individuals (especially children) without body image concerns receive evidenced-based feeding rather than eating disorder interventions. This would help eating disorder researchers refer to the already established treatment for feeding rather than attempting to apply or adapt eating disorder treatments to feeding populations, as has increased just because ARFID was added to the DSM.
Want to learn more?
Check out our lay-friendly article in the Blend mag!:
Check our journal publication on successful brief in-home therapy with a teenager!:
More details on ARFID vs PFD from Feeding Matters: