Services
and direct feeding interventions.
Learn How We Support Severe and Complex Feeding Issues
For more information on the process and to request an intake consultation appointment:
Why early intervention and prevention are important
Why is it important to get proper help? Research highlights the benefits of timely help.
We address the issues that keep your child from eating well.
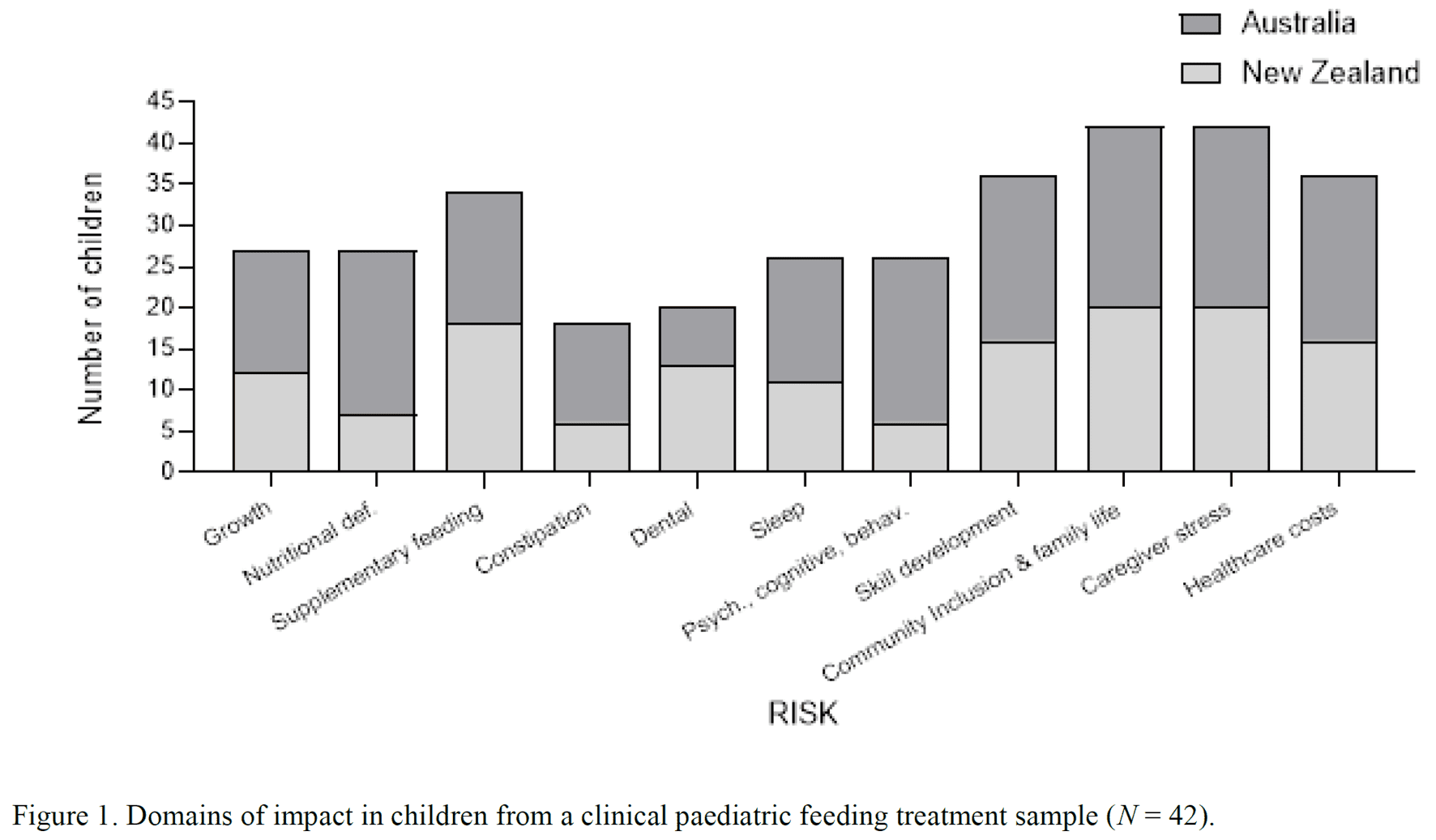
Eating and drinking is vital and one of the most important things we do from birth next to breathing. It occurs multiple times a day and impacts almost all other areas of a child’s development and life; thus, should be top priority. No human behaviour has greater biological and social significance. Without proper support, in severe cases substantial risks to health, well-being, and adaptive skills can arise as complications (e.g., stunted growth, tube placement; impacts on toilet training, sleeping, and talking). (see review by T. Taylor & S.A. Taylor, 2021)
Feeding may be what leads parents to a physician’s office to identify other diagnoses, and paediatric feeding disorders are more prevalent than autism. Substantial risks can be faced by children with paediatric feeding disorders who do not receive timely and effective treatment (T. Taylor & S. A. Taylor, 2021). Feeding problems occur during critical developmental periods for brain and skill development. This can impact a child not only medically, but in most other critical areas of a child’s life and development, including toileting, toilet-training, sleep, learning, behaviour, and severe problem behaviours (e.g., self-injury, aggression, rumination, pica). Feeding problems also have significant impact on social development, participation in community, school, and extracurricular participation, family functioning, and travel. Feeding issues can be a barrier to getting and succeeding with treatment for these other issues until it is resolved; thus, treating the feeding disorder should be prioritised as it can improve the other areas naturally and set the child up for success with other interventions if not. Without appropriate care, children with severe paediatric feeding problems are at risk for dehydration, dental decay, tube placement, growth failure, vitamin and mineral deficiencies, immune system compromise, emergency room visits, hospitalisations, infections, blindness, hearing loss, constipation, scurvy, pellagra, rickets, fractures, fatigue, low strength, behavioural and mental health disorders, sleep disorders, brain function deficits, obesity (and its wide ranging health impacts such as cardiovascular disease, diabetes, and some cancers), disrupted puberty, lower IQ, and death. They also may refuse medications, supplements, and tooth brushing. Developmental delays could impact ability to crawl, walk, and talk, leading to oral, motor, and sensory issues. “Let’s not wait and see: The substantial risks of paediatric feeding problems” (T. Taylor & S. A. Taylor, 2021; International Journal of Child and Adolescent Health).
Pica (eating non-food items) is one of the most serious and life-threatening self-injurious behaviours. Serious risks can include intestinal obstruction and perforation, choking, infection, poisoning, oral and dental health issues, irritable bowels, enlarged colon, constipation, surgery, parasites, toxicity, vomiting, lethargy, gagging, problem behaviour due to blocking (e.g., aggression, self-injury, disruption), and death.
It is not always true that children will eat when hungry if starved, that they will grow out of it (and even if that were true it is still not fine to go through critical developmental years without adequate nutrition and hydration), that they are fine if their weight is fine, that they are not “ready” or able to eat (unless there is a medical safety/aspiration reason) or can’t eat because of a diagnosis, or that attempted treatment is progressing because they are playing with or kissing food but not actually eating it (see review by S.A. Taylor & T. Taylor, 2021). Research has shown the opposite (feeding problems and health and impact becoming worse over time and with age). Thus, if a child is not actually consuming multiple foods from all 4 foods groups of protein, starch, vegetable, and fruit (moving towards age-appropriate texture and independence [self-feeding, drinking]) and drinking water and milk/formula from an open cup within a few weeks (or months at most), he or she needs to be referred for assessment and empirically-supported treatment, and the earlier/younger that occurs, the better (e.g., 1-2 years old). Treatment for paediatric feeding difficulties becomes increasingly difficult as a child gets older, and intervention options and outcomes become limited.
What is the treatment?
Well-Established, Empirically-Supported Treatment with 50 Years of Research
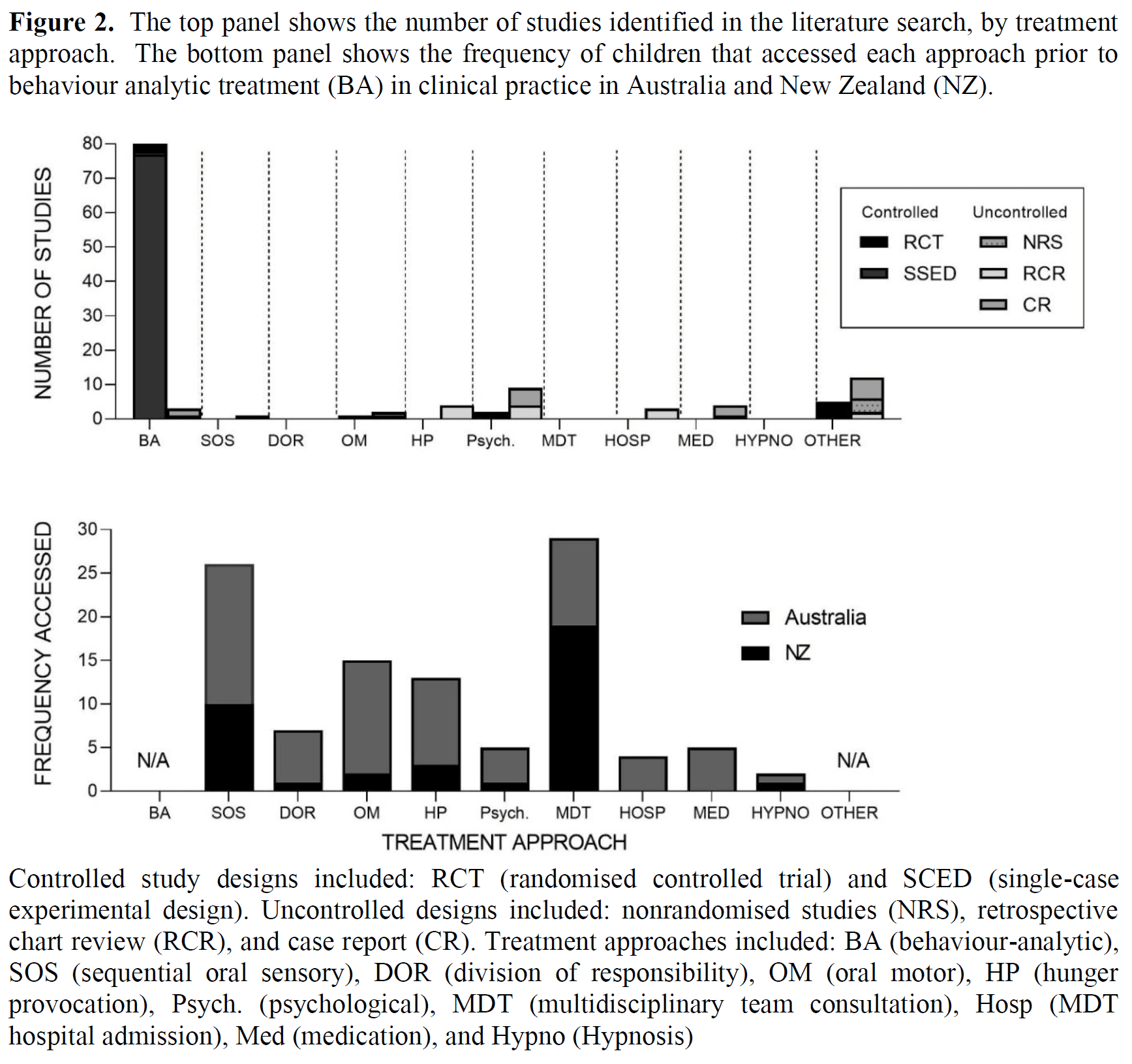
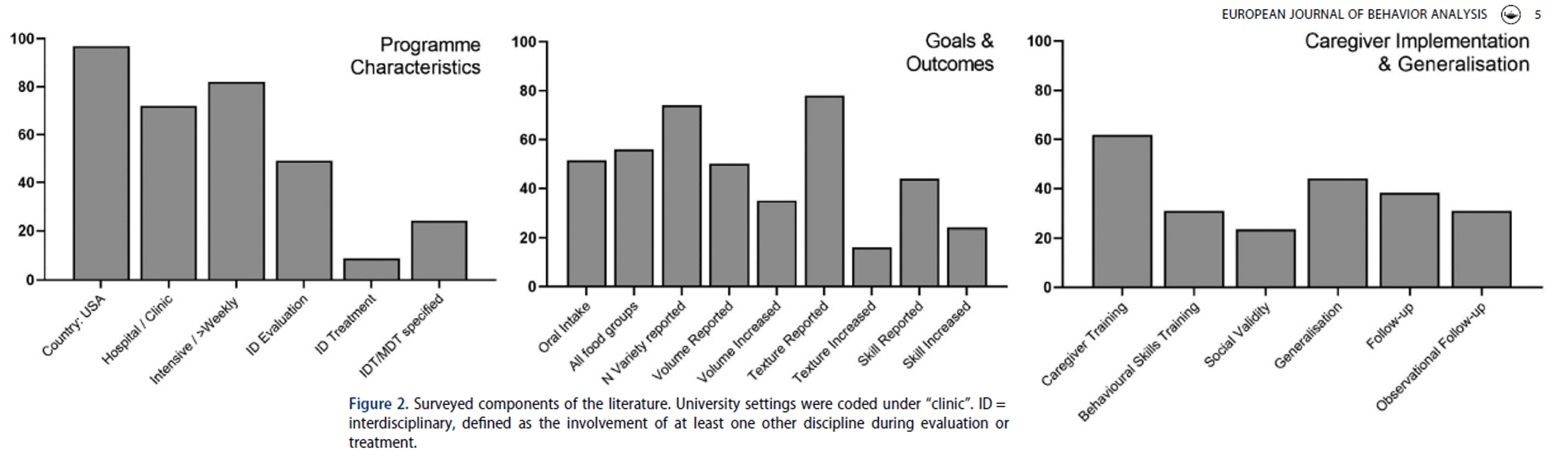
Behavioural approaches are individualised, data-driven, intensive, and use well-established empirically-supported treatments (EST) with 50 years of scientific research to show outcomes (see EST criteria reviews for feeding by Kerwin, 1999 & Volkert & Piazza, 2012, and for pica by Hagopian, Rooker, & Rolider, 2011). See review article by S.A. Taylor & T. Taylor, 2021 reviewed by the Association for Science in Autism Treatment (ASAT) at https://asatonline.org/research-treatment/research-synopses/treatment-for-pediatric-feeding-problems/; & review article by T. Taylor & S.A. Taylor, 2023).
For caregiver-friendly resources: Check out https://www.paediatricfeedingintl.com/resources/.
This intervention requires years of specific training typically available only in a handful of locations in the USA. Families worldwide go for a 2-month hospital admission to Kennedy Krieger’s feeding programme in Baltimore, Maryland, USA, the original model for treating children with severe and complex paediatric feeding disorders. Outcome data (available on their website (https://www.kennedykrieger.org/patient-care/centers-and-programs/feeding-disorders-program) show that children meet over 90% of individualised goals and caregivers report high levels of satisfaction (https://www.kennedykrieger.org/outcome-data-2023/feeding-disorders-program). Anecdotally, children who had never ate by mouth had gastrostomy tubes removed and could now attend a regular daycare or school (versus a special one for tube care) and ate their first birthday cakes (even if they were 7 years old) or Thanksgiving dinners and participated in holiday traditions. Children ate for the first time on vacation with their families or at parties or at school with their friends, had enough energy to participate in sports, learned to chew and take bites independently despite being told they were not able, went to camp overnight, and parents who had battled mealtimes for years were able to feed their child family dinner without getting the exact same takeout everyday prepared in a certain way. This can be a lifechanging trajectory for the family and the child on multiple levels (e.g., medical, social, developmental, monetary). *individual results may vary.
This approach does not require extreme deprivation of tube nutrition or preferred foods/drinks initially (i.e., starvation/hunger provocation). Throughout the programme, changes are made quickly and continue until intervention works and the child is eating*. Therefore, vital nutrition is not withheld or delayed during critical developmental periods for children due to deprivation or lengthy (e.g., years, months) interventions not targeting actual eating/consumption. This intervention also teaches skills needed for age-appropriate independence in eating and drinking, and that children eat a balanced, nutritional diet from all 4 food groups at the most age appropriate texture possible. This approach can work regardless of diagnosis, ability/skill level, or tube status, and should be implemented as early/young as possible. It is tailored to each child by direct work with the child to find out what works, and then caregivers are helped and trained thoroughly on precise, already proven procedures specifically for their child so that they can do it alone once the programme is finished. Many children have received years of costly prior attempts, including intensive interdisciplinary hospitalisations, “desensitisation,” medications, supplements, hunger provocation/starvation, speech/occupational/psychological therapy, oral-motor and sensory therapies, and consultation with teams, dietitians, and other medical professionals. This approach is individualised specifically for each child’s particular feeding needs, as opposed to generic advice for parents to try. *treatment duration varies per individual and is tailored to each child’s specific needs; individual results may vary.
Behavioural feeding treatment can reduce caregiver stress, increase child happiness, have a positive impact on child emotional and behavioural functioning, and not negatively impact the quality of the mother-child relationship/attachment; additionally, caregivers report high satisfaction and rate the treatment highly positively with no negative side effects in follow-up, in addition to the rippling positive impacts of intervention extending beyond eating for the child and family (e.g., see systematic review (of 26 studies) by Taylor, Phipps, Peterson, & Taylor 2024, with 3 other colleagues from 4 different sites across 3 countries). *individual results may vary.
For full text research articles on empirical support for this approach and comparison studies to other approaches, and our feeding and pica treatment articles: Check out outcomes from transitioning this treatment to Australia https://paediatricfeedingintl.com/success-stories/ (Taylor, Blampied, & Roglic’, 2020; Taylor & Taylor, 2022).
How does the programme and treatment work?
Intake can be completed either in-home or with video conferencing remotely. A physician has to complete a clearance form. A comprehensive evaluation is done in coordination with the child’s team as needed (e.g., gastroenterologist, paediatrician, allergist/immunologist, speech pathologist, other therapy providers) to evaluate medical, safety, and skill issues and if referrals and/or testing are needed. We watch your child eat and drink directly to observe skills and mealtime behaviour. Intensive in-person treatment can be provided for children 5 years and younger. Together, we set measurable individualised goals. Treatment services are mobile and provided in-home worldwide. Treatment is intensive (multiple full days in a row) depending on your child’s needs, severity of feeding problems, and goals. This allows for high family schedule flexibility because we only work with one child at a time. Your child will have frequent breaks throughout the day and a lunch break. In each session, we use a special realtime laptop programme to measure your child’s progress. We take pictures of the food they eat and weigh it in grams. A trained assistant is present through the programme. All sessions are videoed and Dr. Taylor (ClinPsych) can watch the videos with you and discuss your child’s progress. We directly assess your child’s preferences and what changes we can make to increase mealtime performance. An individualised treatment is systematically evaluated using a data-based approach. We especially evaluate what your child needs to succeed in meals. Goals include increasing variety and range of foods, increasing amount (volume) in meals, increasing food texture, teaching cup drinking, teaching chewing, increasing self-feeding/drinking, teaching scooping, opening and closing on the spoon, biting off food portions, accepting medicines and vitamins, etc. Treatments are individualised and data-driven, and involve changing the mealtime environment, such as providing incentives and rewards for swallowing and praise, setting achievable mealtime requirements and gradually increasing them, continuing to present food and liquids, replacing food or liquid spat out, providing instructions, guidance, and help, and teaching the skills needed to achieve goals. For example, we provide children with choices and their favourite items and activities such as music, videos, or toys, and give rules and instructions and show children how to do the skills such as chewing and using a spoon. Once treatment is successful, we directly help you to learn to do it yourself with your child with individualised support; thus caregivers must be present during the majority of this process. Dr. Taylor can sign a letter for you to take off of work or school. Training includes watching meals, reviewing a written protocol and cheat sheet, practising with Dr. Taylor before feeding your child, and gradually working into actually feeding the meal yourself with help, then coaching via phone/video conferencing with Dr. Taylor out of the room, coaching via video review of meals alone, etc. Hours of treatment are decreased as you are able to feed more independently. Close follow-up support as needed is provided to ensure ongoing progress and success. Other caregivers and school and daycare personnel can be trained as appropriate. We can do meals out at restaurants or school, or with extended family and siblings. Follow-up continues for two weeks after the programme with video conference meals as needed, and for all meals, video and plate picture review and shared data collection and communication.
For more information for families on what to expect on the hospital programme this is from, go to https://www.kennedykrieger.org/sites/default/files/library/documents/patient-care/patient-care-programs/outpatient-programs/14102_2018FeedingProgramHandbookReprint_IA1.pdf
How much does it cost?
A Cost-Effective Treatment
Aside from the significant medical, social, developmental, and familial benefits of successful treatment for paediatric feeding disorders, the cost effectiveness of intensive treatment has been demonstrated (Dempster et al., 2015 & 2023, Piazza and Carroll-Hernandez, 2004, Serban et al., 2020, & Williams et al., 2007) in USD. Dempster et al., (2023) found children who received treatment had decreased health care charges by 71% compared to increasing charges by 22% if not. Dempster et al., (2015) reported a cost of $56,946 for gastrostomy tube placement surgery, $24,127-$26,737 (5-10 years) for tube removal, and calculated average routine maintenance costs (e.g., pumps, bags, tubes, formula) over 5 years at $202,095 and 10 years at $376,424. Williams et al., 2007 calculated that yearly routine maintenance costs could reach $70,889. These figures do not include other variables such as complications, medical appointments, emergency room visits, hospitalisations, specialised daycare/school placements and nursing, etc. or the high costs of months and years of ineffective therapies and hospitalisations most children receive before obtaining evidence-based treatment. Cost savings for a 70% (which is low/conservative compared for the evidence) to 100% success rate for tube removal at 5 years is $94,635-$122,412 and at 10 years is $266,353-$294,131, and for tube prevention at 5 years is $172,681-$200,459 and at 10 years is $344,400-$372,177. In addition to gastrostomy tube costs, additional costs can be incurred for children with failure to thrive, including nutritional deficiencies, hospitalisations for dehydration or temporary tube placements (e.g., nasogastric supplementation), oral supplements and formulas, constipation, specialised placements for school/day-care, dental decay, blindness, etc. Even in the US with insurance, families managing paediatric feeding disorders (PFD) face significant financial hardships and emotional tolls, and the economic burden is immense e.g., lost income of $125,645, plus supplies, travel, time, cost coping strategies, treating personal stress, and psychological care (Feeding Matters, 2019). Disclaimer: This research is from the USA where the healthcare system differs; Australia does not have this research on PFD, but see articles by the Butterfly Foundation on Paying the Price and Investing in Need for eating disorders e.g., $80.1 billion and a ~5:1 cost/benefit ratio of appropriate and timely treatment.
Families worldwide go for example to Baltimore for a 2-month hospital admission, and private and public health insurances in the USA provide coverage for this treatment*. Although this may appear to be a high lump cost estimate, many children we see have exceeded this cost long-term over weekly appointments for multiple years. The goal of this approach is for the family to be given what they need for the child to eat/drink with them and eliminate need for more services and costs, with exception of kids who need more time to build their skills (e.g., chewing) or handle larger volumes. This short-term intensive intervention can resolve the feeding issues as long as the family keeps it up (with possible exceptions e.g., acute stomach illness, mouth surgery, new feeder needs training, severe cases with further skill development/time needed with chewing, self-drinking, scooping, biting off, etc.). A couple week to month programme that can resolve the issue long-term and eliminate service need is valuable.
The cost of this programme varies as intensity of services is individualised and depends on response to intervention/progress which is data-based. The total actual cost of services is based on actual hours delivered rather than the estimate. Caregiver training and fading of hours will begin as soon as possible depending on progress made and goals met. Some children graduate early and cheaper than the estimate. Some kids take longer.
*Note: This is funded in the USA by most private insurance companies and Medicaid (and more expensive). There’s a long history of successful appeals and overturned decisions from the past in the USA that has established this. Please see Hagopian et al., 2015 for references for judicial rulings, legislation, and insurance reform. Full text articles on cost-effectiveness